Frontiers in diabetes patient management
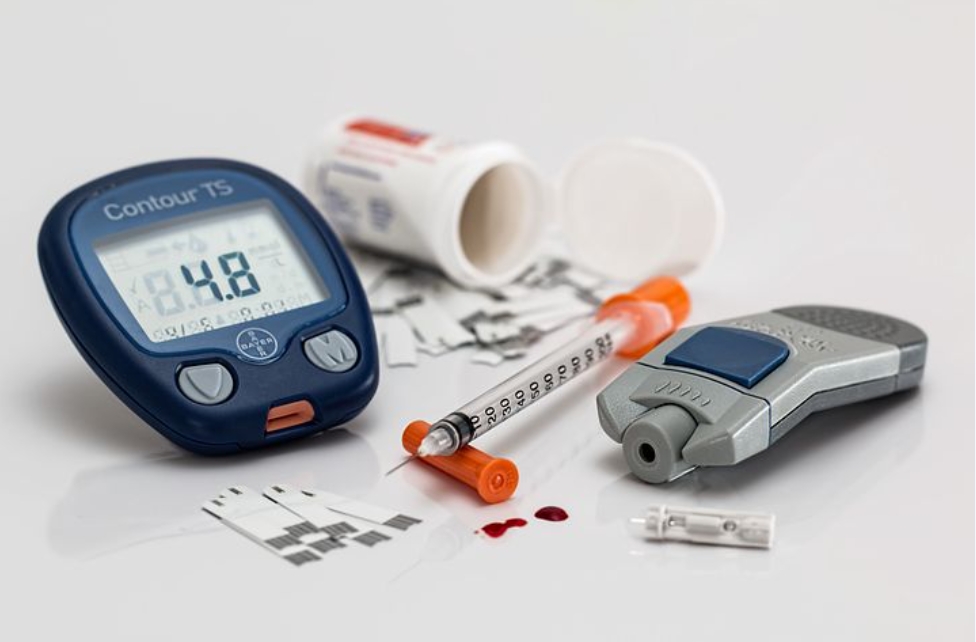
COVID-19 has posed both obstacles and opportunities for diabetes management and technology since the advent of the pandemic. The health crisis of COVID-19 has highlighted the value of providing technology that lets medical professionals quickly recognize their diabetes patients and check their commitment to monitoring and office visits. Before the pandemic, many patients with diabetes were already using technology on a regular basis, such as the use of insulin pumps and continuous glucose monitors, as well as 'smart' glucometers or insulin pens, which have increased dramatically in recent years. The diabetes patient and disease management in COVID-19 should not only be restricted to self-care by patients but also hospitals, clinics, and all the healthcare providers should take the responsibility to monitor and manage blood glucose levels, follow-up routines. If these care are not provided on time or properly, there could be an increased risk of not just long term-complications such as heart and kidney disease and vision and nerve problems, but short-term, potentially life-threatening problems such as severe low blood glucose levels or diabetic ketoacidosis.
During this age, the use of telehealth has been immensely beneficial in ensuring safe and continuing care for patients. Physicians have been able to access their patients by using Facetime and Google Duo, among other common video communication channels, with[the Health Insurance Portability and Transparency Act] easing their rules and regulations. The use of this technology and telemedicine remains in place with sufficient insurance coverage so that doctors and patients can continue to communicate in a more modern and open way. Remote monitoring offers patient health insight in real-time, helping physicians to identify patient deterioration early and to intervene to prevent severe health problems. This may mean preventing serious hospitalization incidents such as diabetic ketoacidosis or hypoglycemia for patients with diabetes by identifying early signs of changes in pulse and respiratory rates and glucose derangement.
Since patients respond to various channels of communication differently, doctors should consider a range of patient-connecting technologies. Phone calls can be suitable in some situations. Safe texting, email, or secure messaging can be better referred to by other patients. Smartphones offer a huge opportunity to better communicate doctors with their patients, but the smartphone has been prevented from being the gold standard in physician-patient contact by a variety of legislative, access, and acceptance barriers.
A combination of human contact through competent clinical coaching and experience with different technology must be incorporated into the most successful remote management strategy so that patients understand how their devices function and care teams can respond to any "red flags" detected either by the participant or by an irregular laboratory value transmitted by their computer.