The Importance of Surgical Staging in Differentiated Endometrial Cancer: Findings from a Sri Lankan Study
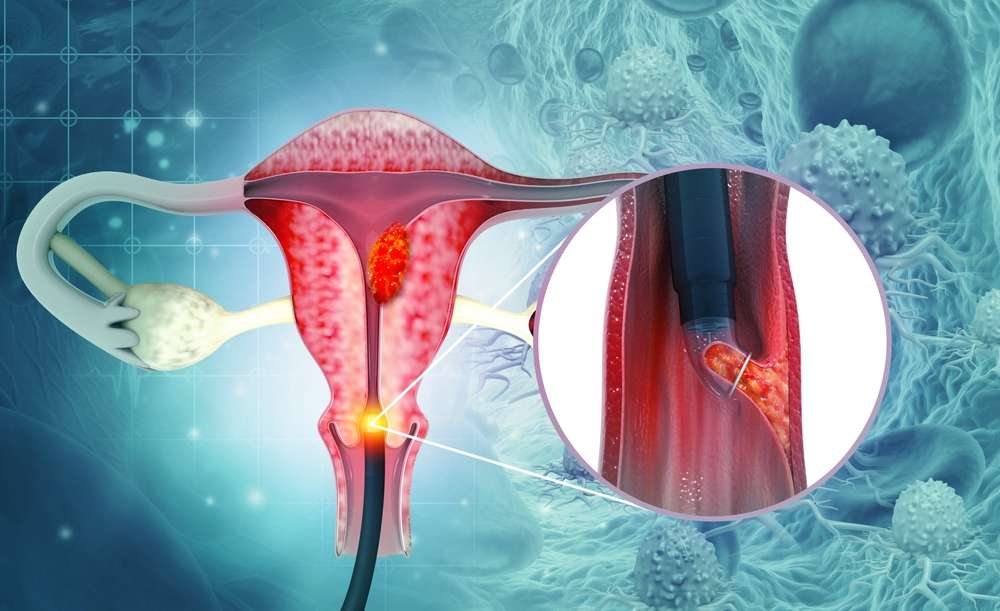
In this study conducted in Sri Lanka, the management of differentiated endometrial cancer and the role of surgical staging were evaluated. While surgico-pathological staging is recommended for poorly differentiated endometrial cancer, the controversy lies in the management of well-differentiated cases. Limited access to preoperative pelvic and abdominal Magnetic Resonance Imaging (MRI) in Sri Lanka makes surgico-pathological staging the primary method for most patients.The objective of the study was to assess the outcome of surgical staging among differentiated endometrial cancer patients who underwent primary surgery at a gynecological cancer center in Sri Lanka. The study analyzed data from December 2019 to December 2020. Among the 90 patients with differentiated endometrial cancer included in the study, 60% had medical comorbidities. It was found that 35% of patients had myometrial invasion of more than 50% thickness. Interestingly, patients with deep myometrial invasion had a higher likelihood of lymph node metastasis compared to those with superficial or no myometrial invasion.The study concluded that approximately one in seven patients with deeply infiltrating differentiated endometrial cancer had lymph node metastasis. In settings where preoperative pelvic MRI is not readily available, implementing a policy of routine surgical pelvic lymph node assessment would be beneficial. This approach would aid in detecting stage IIIc disease and also help avoid unnecessary pelvic irradiation. This study sheds light on the importance of surgical staging in differentiated endometrial cancer and highlights the need for alternative methods in limited resource settings. By identifying patients at risk for regional metastasis through surgical staging, appropriate treatment plans can be devised, leading to improved outcomes for these patients.
To know more: About the original article click here.
