Mucormycosis after COVID 19 in a patient with diabetes
Recently, there has been an increase in the number of mucormycosis after COVID-19 infection, especially in patients with diabetes. This is a descriptive study conducted at the only COVID Treatment Center in India in patients with COVID-related mucositis from April 12, 2021, to May 31, 2021. COVID 19 infection. The incidence was 3.36%. Among patients with CAM, 87.5% of the most frequent comorbidities were diabetes.
A 44-year-old man came to our hospital and said that his vision in his left eye had deteriorated.10 days earlier, he began treatment with supplemental oxygen, intravenous antibiotics and corticosteroids for moderately severe pneumonia caused by SARSCoV2.
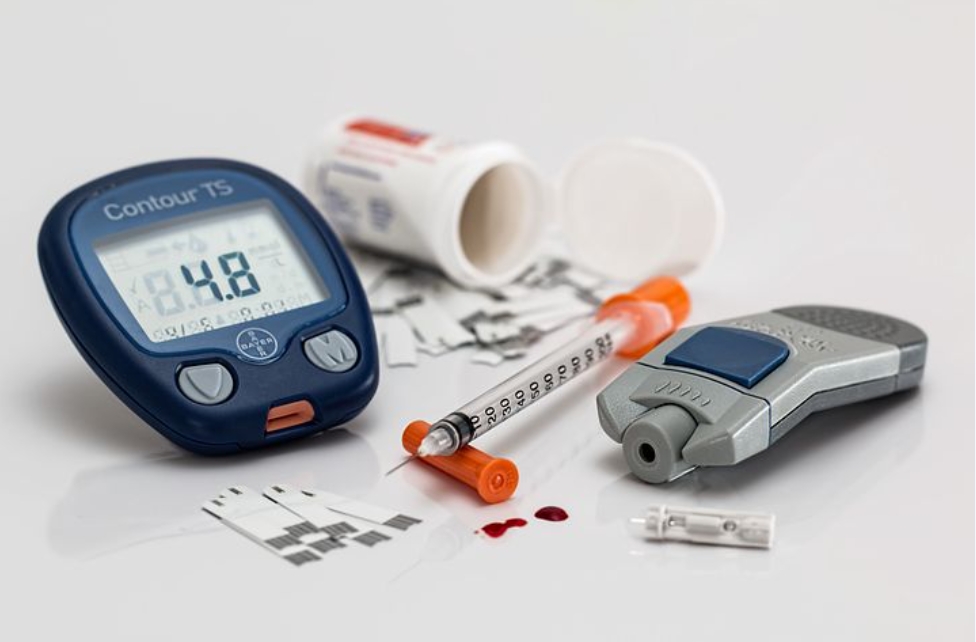
The patient explained that a dark spot had appeared two days earlier, extending from just below the left eye to the left side of the face and at the level of the mouth. The patient is known to be diabetic; There was no history of malignant neoplasms. On examination, the temperature is 37 ° C, the pulse is 84 beats/min, the blood pressure is 118/82 mm Hg. Art., Respiratory rate 16 beats/min; Pulse oximetry showed 96% oxygen saturation in the ambient air.
The patient was admitted with bulging eyes, eye pain and chemoradiotherapy in the left eye. The best-corrected visual acuity in her right eye was 20/20, but she did not report light perception in her left eye. Laboratory tests revealed a random blood sugar level of 298 mg / dL, glycated haemoglobin A1c 9.8%, arterial blood pH 7.4, serum bicarbonate level 24 mEq / L, and mild leukopenia.
A study of preparation of potassium hydroxide from a nasal swab revealed a wide mycelium, pauciseptate; and culture on Sabouraud dextrose agar and lactophenol blue cotton attachment showed Rhizopus arrhizus.
Contrast magnetic resonance imaging does not show bi-directional amplification of the middle and lower turbine: characteristic black turbine mark.
An unimproved area of adjacent soft tissue was noted in the left ethmoid cell and medial gas cell with a cleft ethmoid plaque enclosing the anterior basal region.
T2 Intense diffuse inflammatory changes were observed in the soft tissues of the left orbital region about the anterior, posterior, and also intra- and extra-compartmental regions with orbital fatty fibres.
Unevenly increased inflammatory changes in soft tissues were observed on the left side of the face, including the premolar region, pterygium, and thoracic concavity. In general, the clinical picture and radiological data indicate mucormycosis. The patient started treatment with liposomal amphotericin B intravenously at a dose of 5 mg/kg per day; Insulin infusion was also continued due to persistent hyperglycemia.
Large excision, maximal left resection, and orbital reconstruction were performed under general anaesthesia; however, the patient died after 6 days.
During the second wave of the COVID19 pandemic, India saw an unprecedented increase in mucormycosis: immunoregulatory dysregulation of SARSCoV2 and use of broad-spectrum antibiotics and corticosteroids, especially in patients with poorly controlled diabetes mellitus with ketoacidosis increased. SK and DSA provided clinical diagnosis and patient care. SK and KC recommend manuscript and patient follow-up.
Written consent for publication was obtained from the patient’s immediate family.
In diabetic patients affected by COVID19, superinfection with mucormycosis is associated with poor clinical outcomes and prolonged hospital stays. This study aims to investigate the clinical spectrum of mucormycosis after COVID19 and diabetes and its subsequent outcomes.
Treatment and progression Patients in our centre were started treatment with liposomal amphotericin B to control blood glucose due to clinical suspicion of mucormycosis, followed by endoscopic resection. Most patients, 21 of 32 CAM patients, had COVID syndrome after clinical recovery from COVID19.
In Western countries, diabetes is associated with 17 cases of mucormycosis. The incidence of mucormycosis is about 1.6 cases per 1000 patients with diabetes mellitus. Mucormycosis is a group of life-threatening infections caused by fungi of the order Mucorales, subclass Mucoromycotina. An increasing incidence of mucormycosis due to infection with Cunninghamella spp. Has also been reported, especially in severely immunocompromised patients.
Rare case reports have demonstrated the ability of fungi from the remaining Mucorales families to cause mucormycosis, although other Mucorales species may be a major cause of disease in certain geographic areas. Patients with elevated levels of free iron, which promotes the growth of fungi in serum and tissues, are also at risk of developing mucormycosis. Most diabetic patients with mucormycosis are not acidophilic, and even in the absence of acidosis, hyperglycemia directly increases the risk of mucormycosis by at least three possible mechanisms: increased saccharification of iron sequestration proteins, impaired normal iron sequestration. Iron; regulation of receptors of mammalian cells that bind to Mucorales, allowing penetration into tissues; and cause poorly characterized defects in phagocytic function.
A month after India reported the first case of mucormycosis after the second wave of the novel coronavirus pandemic, many theories have emerged as to the reasons for the increase in rare fungal infections.
India’s mucormycosis infection rate is 70 times higher than in the world, even without the consequences of the second wave of COVID19. Mucormycosis in India after the second wave of COVID19. An earlier version of this document, scheduled for publication in September 2021, recorded a 2.1-fold increase in mucormycosis cases in India during September-December 2020 compared to the corresponding period in 2019. The order of mushrooms is called “dematiaceae”. ; it has nothing to do with mucormycosis.
Trichiasis is not as dangerous as mucormycosis and mainly causes infections under the skin or the nails. What distinguishes mucormycosis from other fungal infections is that it spreads quite rapidly – 4 and 5 centimetres a day, mechanistic researchers say.
Mucormycosis can be fatal if left untreated. Mucormycosis is a fungal infection that mainly affects people taking medications for other health problems that reduce their ability to fight environmental pathogens.