Diabetes management could help reduce the overall burden
Diabetes is one of the most prevalent non-communicable illnesses related to increased morbidity, mortality, and economic burden. In 2015, an estimated 415 million humans have been living with diabetes mellitus (DM) and the variety is predicted to rise to 624 million by 2040. This boom is in parallel with the global developing epidemic of obesity, in addition to the populace growth and aging. Diabetes is likewise an expensive disease with a wonderful financial burden on affected humans and health care structures, mainly in low- to middle-income countries (LMICs) due to its durability and severe related macrovascular and microvascular complications. In 2013, 77% of patients with diabetes (382 million) lived in LMICs. Moreover, the projected boom in occurrence is better in low-earnings countries (108%) and LMICs (60%) as compared to upper-center countries (51%) and high-earnings countries (HICs) (28%). The rate of growth is inversely associated with the countries’ earnings status and has been attributed to the speedy urbanization accompanied by the adoption of sedentary existence and unhealthy dietary habits. Another exciting locating from this evaluation became that younger or underweight people with diabetes in those settings had worse overall performance than older and overweight/overweight people in phrases of rates of testing, carrier utilization, and diabetes control. This locating suggests the want for mainly guiding screening and reinforcing linkage to care in those unique subsets of populations. In an observation from Seychelles, at the national level in a random sample of 1,255 participants, it was observed that only 54% of people with diabetes were aware of the diagnosis. While treatment was offered in 98% of them, out of them only 21% had satisfactory diabetes control. A population-based study in Malawi, enrolling 28,891 adults (≥18 years) residing in two defined geographical areas, also reported 59% of people with diabetes being diagnosed, out of whom 62% being treated and only 41% of those under treatment achieving adequate control In 2019, an analysis of health systems’ performance of diabetes management across 28 LMICs in multiple geographic regions from nationally representative population-based surveys was performed. In this analysis, data collected from 2008 onward were included and analyzed by a cascade of care analyses. It also reported that health system performance for diabetes management in low-resource settings is generally characterized by large losses to care at the stage of diabetes testing and only moderate rates of diabetes control.
In conclusion, during the last years, we’re observing an epidemiological transition in LMICs. Non-communicable diseases which include DM are expected to overtake infectious diseases, maternal/toddler mortality, and malnutrition with the aid of using 2030. There is an important window for the improvement and implementation of effective diabetes care fashions in LMICs. These fashions can function as a stimulus for the alternate in delivery and receiving hospital therapy in LMICs, and diabetes can function as a capacity tracer for reexamining health structures in those countries. Diabetes health care fashions must goal growing patients’ access to care, schooling sufferers and neighborhood fitness care professionals, standardizing tips for prevention and management, and the usage of technological innovation to enhance the effectiveness of care furnished and health outcomes globally.
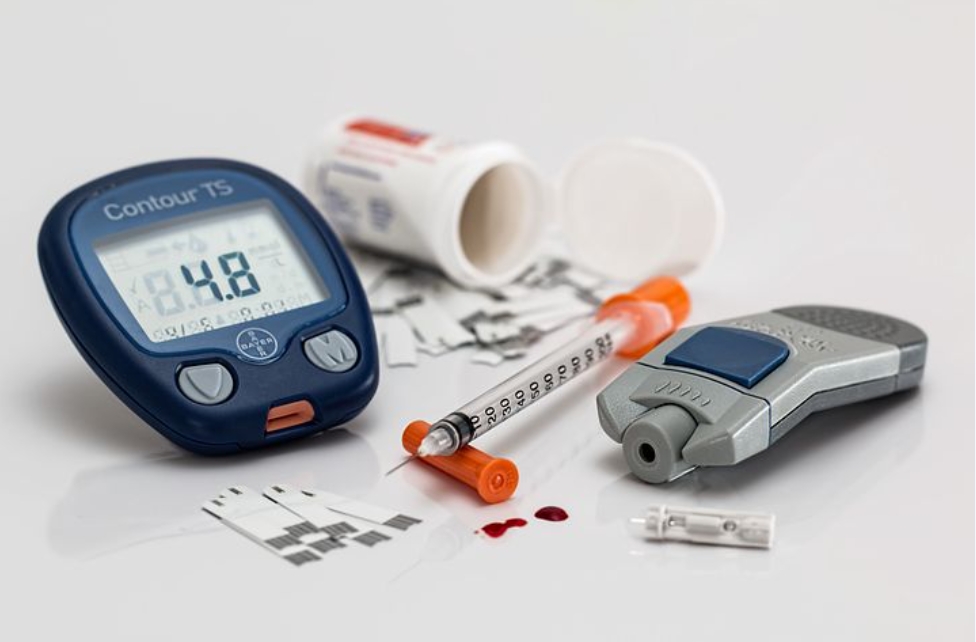
Photo by Diabetesmagazijn.nl on Unsplash